The topic of imaging in musculoskeletal medicine is vast and not likely to be fully covered in this article. It is however important to discuss the various indications for modalities and where they fit in the diagnosis of your clinic patients. We now live in an age where most patients are well informed and often will present requesting an MRI scan as an initial step in management. Whilst at times this may be appropriate often there may be another test which is more appropriate. We know there will be a cost to the patient and community in terms of money and time to obtain the test. Medicare spends millions of dollars every year on subsidising the costs of investigations, so it is important to order them in the most effective fashion possible. This article will discuss some of the principles of ordering investigations appropriately.
The investigation should change or influence your management.
This is an important concept to ponder anytime you consider getting any test performed. Is the test worth getting and will it change our management? The basis for treating any musculoskeletal condition is founded on accurate diagnosis. Any investigation incurs not only cost (patient/Medicare), but also a time cost to that person, so it needs to be helpful to the treatment of that patient. There may also be a potential for a false positive result which may lead to the need for further investigation and unnecessary treatment. Practitioners must be prepared to manage based on the test result, or there is little point proceeding with the investigation.
The investigation should be the most appropriate one to diagnose the issue based on clinical (history and examination) presentation
There should be a consideration of all manner of imaging relevant to the patient before a modality is chosen. This will be driven by the history, but more importantly the examination. The test should always try to confirm the clinical suspicion, not make the diagnosis on its own.
The investigation should be the simplest (and cheapest) one to confirm the clinical suspicion.
Cost is important when ordering investigations. An X-ray is a much simpler and cheaper test than an MRI, and in many cases may provide all the information that is required to make a diagnosis, without requiring a more ‘high-powered’ scan.
X-ray
There is never a reason to not investigate a musculoskeletal condition initially with a plain X-ray. An X-ray will convey important information with respect to bone and joint issues, particularly osteoarthritis, and assess for the unexpected, such as a cancer. Stress or weight-bearing views may also provide important information in joint instability, such as in a Lis Franc sprain in the foot. If a patient has been treated a few times for any issue and progress is not being made, then a plain X-ray should be mandatory before continuing further physical treatment. A plain X-ray is always helpful, even if normal, and should be provided prior to any specialist appointment either from the referring physio or GP.
Ultrasound
As a rule, ultrasound is an overutilized modality. Whilst it can provide information in certain conditions, a proportion of these can be diagnosed purely on clinical grounds, such as tennis elbow or plantar fascitis. The difficulty with US and tendinopathy, especially with increasing age, is the likelihood of age-related degenerative changes that are not always clinically significant. US also lacks the accuracy of MRI, especially with deeper tissue structures, and can be heavily dependent on not only the operator and reporter, but also the quality of the machine. One advantage of US can be the dynamic nature of the test, allowing assessment of the abnormality with motion in real time. An US should always be ordered in association with a plain X-ray of the corresponding area.
CT scan
CT scanning is most useful for assessment of bony structures and plays little role for soft tissue injury. It can be helpful for diagnosis of missed fractures as an extension of plain X-ray when there may be some doubt on the extent of injury. It offers little above plain films for the diagnosis of osteoarthritis. A downside of CT scanning is the radiation dose, which is significant, especially if performed axially. This is an issue with lumbar scans ordered without a clear history of radiculopathy, which often occurs in the management of lower back pain.
Nuclear medicine (Bone scan)
Whilst nuclear medicine imaging has been replaced in many areas by MRI, it still has a role to play in certain circumstances. Its main advantage is sensitivity, but not necessarily specificity. It may be helpful in diagnosing missed fractures or stress fractures may, but MRI is generally as sensitive for this purpose. With multiple joint issues bone scanning also has the ability to look at the ‘whole body ‘at the one time, with one scan. Bone scanning also has the advantage over other modalities in localizing specific pathology in the presence of wide-spread degenerative disease. This may be helpful with generalized facet joint arthrosis in lumbar spondylosis. It can allow local treatment such as cortisone injection to be performed with improved accuracy.
MRI
MRI is clearly the pinnacle of imaging. It has been described by radiologists as the ‘test of truth’ because there is little that will not be picked up by this modality. In many ways this can be to its detriment, particularly in the older patient, where multiple age-related changes need to be correlated to clinical findings. As such the interpretation of the MRI is just as important as the scan findings themselves. Abnormalities such as labral tearing in the hip, meniscal tearing in the knee and disc desiccation in the lumbar spine do become more common with age and are often incidental findings not relevant to the clinical presentation. MR’s strength is with soft tissue injury and its weakness is with bony injury and particularly fractures, where CT is superior. It is, however, quite sensitive in detecting bone marrow oedema or ‘bone-bruising’.
The major downside with MRI scanning is cost. An MRI is many times more expensive than a plain X-ray and some justification needs to be made for its use from a health economic point of view. It is most beneficial when other modalities have failed to provide an accurate diagnosis or there is ‘diagnostic doubt’.
Common Imaging Issues
Ultrasound of the shoulder without a plain X-ray.
The shoulder is a complex joint with multiple potential causes of pain that may not be related to sub-acromial bursitis, which is a very common finding on US, and often not the clinical issue. X-Ray can adequately assess for osteoarthritis of the AC or glenohumeral joints, acromial morphology, superior humeral head migration and tumours. As previously mentioned, an ultrasound should not be performed without an X-ray of the corresponding body area.
Sub-acromial bursitis is a very common finding on ultrasound. This is a good example of when reliance on imaging over clinical examination can cause issues. Patients may be sent for sub-acromial cortisone injections based on the ultrasound findings when the clinical diagnosis shows restricted shoulder motion, more consistent with an adhesive capsulitis
 Fig 1. Subacromial bursitis in a patient with clinical adhesive capsulitis
Fig 1. Subacromial bursitis in a patient with clinical adhesive capsulitis
Ultrasound of the knee.
As a modality around the knee US does have limited indications. It will not diagnose meniscal tears or osteoarthritis. Knee effusions should be detected clinically, as should knee instability. Baker’s cysts are generally an incidental finding related to osteoarthritic change. If there are concerns about intra-articular pathology in the knee and X-rays are normal, then an MRI is the most appropriate test.
Ultrasound of the hip without a plain x-ray
As with the shoulder, an X-ray of the hip should be a mandatory test if an ultrasound is performed. The most common cause of groin pain, particularly in the older patient, is underlying hip joint osteoarthritis. This will not be diagnosed on ultrasound alone and should be apparent on a hip and pelvis X-ray
 Fig 2. Hip osteoarthritis in a 60-year-old man with groin pain
Fig 2. Hip osteoarthritis in a 60-year-old man with groin pain
CT scan of the lumbar spine
As a rule, CT scans are an over ordered investigation for lower back pain, particularly by general practitioners. In simple non-radicular back pain often no imaging is required, or at best a plain X-ray if symptoms are not improving after appropriate treatment, or there are any ‘red-flags’. Plain X-ray will exclude any sinister pathology and can assess for disc desiccation and facet arthrosis. CT scanning is indicated in radicular pain, but does lack accuracy in comparison to MRI, which should be the investigation of choice. It also carries a significant radiation dose, which MRI does not.
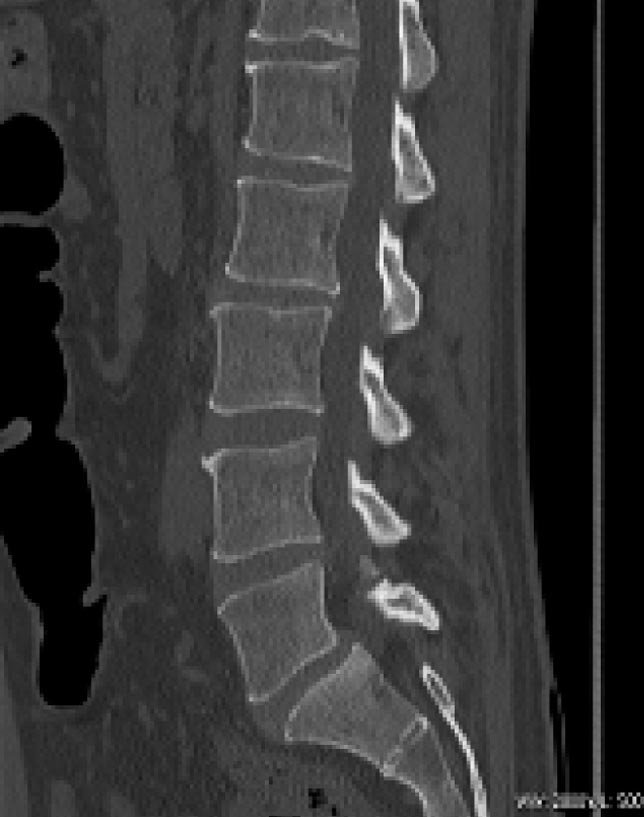 Fig 3. CT scan showing lumbar spondylosis in a patient with non-radicular lower back pain
Fig 3. CT scan showing lumbar spondylosis in a patient with non-radicular lower back pain
